If you watch television on a regular basis, you have undoubtedly seen ads for a variety of prescription and non-prescription drugs to reduce or eliminate the symptoms of heartburn, one of the fastest growing medical complaints in today’s fast-food, stress-filled world. Yet many of us are unaware that heartburn, especially chronic heartburn, is often associated with a serious medical problem called gastroesophageal reflux disease (GERD), also sometimes called acid reflux disease.
Those of us suffering from acid reflux disease, which is related to the inappropriate relaxation of the lower esophageal sphincter, will be interested to know that how we breathe may well influence this disease. A study published in The American Journal of Physiology (May 30, 1995), for example, discussed the relationship of partial expiration and hyperventilation on the gastroesophageal junction. The abstract of the study concluded by stating: “The breathing patterns of partial expiration and hyperventilation have significant influence on esophageal motor function. Abnormal breathing pattern may be involved in the pathogenesis of esophageal motor dysfunction.”
Another study at the Department of Internal Medicine at the University of Virginia at Charlottesville concluded that the inhibition of the “crural diaphragm during transient lower esophageal sphincter relaxation may play an important role in facilitating flow across the gastroesophageal junction.” In other words, there is some evidence that an overly tight crural diaphragm (the part of the diaphragm composed of muscular strands that attach to the lumbar spine) causes inappropriate relaxation of the lower esophageal sphincter.
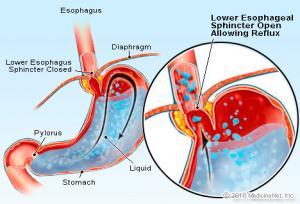
To understand the possible significance of these studies with regard to the way we breathe, it is important to remember, first of all, that the esophagus traverses an opening in the diaphragm to reach the stomach, and that there is a sphincter at the entrance to the stomach that must relax for the food we have eaten to enter the stomach. Relaxation of this sphincter takes place mainly when we swallow and when food is traveling through our esophagus into our stomach. Relaxation of the sphincter at other times allows a flow from the stomach upward, which can cause inflammation of the esophagus and throat. If left untreated, ongoing inflammation can have many serious effects on our health, including ulceration and cancer of the esophagus. These studies seem to suggest that poor breathing habits, including chronic hyperventilation and incomplete exhalation, may well be involved in acid reflux disease.
If you do have acid reflux, it is imperative that you work to improve your breathing. The key is to learn how to exhale as completely as possible and to breathe with more of your whole body, especially your belly. An excellent first exercise is the belly breathing exercise on this website. Other helpful practices can be found in my books.
Special Note: There are two supplements that we recommend that may be helpful for people with inflammation of the digestive tract:
One is Dyglycyrrhizinated Licorice (DGL), which you can find in most health food stores. Regular licorice also has soothing effects on the GI tract, but it is not advised for anyone with high blood pressure. DGL apparently does not influence blood pressure.
The other supplement is omega-3 fatty acid, especially ultra-refined fish oil. Those with GI tract inflammation would be wise to look into the work of Dr. Barry Sears, who discusses the importance of insulin control as well as the importance of high-dose fish oil in combating inflammation, in his book The Omega RX Zone. Sears maintains that the fish oil found in health food stores is not pure or potent enough to be used in the high doses required to treat serious inflammation. Learn more about the importance of ultra-refined fish oil.